
Gymnastics Medicine founder Dr. Elly Hart on what to do if you are experiencing back pain in gymnastics.
Back pain is NOT normal for any gymnast or athlete to have. Any gymnast who experiences acute (an injury from a fall or awkward landing) or chronic (long lasting and without a specific fall/injury) back pain should be seen and evaluated by a medical provider.
The incidence of back pain in gymnasts ranges from 25-85% (1) and one study found that for women’s collegiate sports, gymnastics had the highest rate of back pain compared to all other women’s sports (2). Risk factors for having back pain include, but are not limited to, abdominal muscle weakness, tightness with hip extension, shoulder flexion, and thoracolumbar fascia, increased femoral anteversion, genu recurvatum (hyperextended knees), increased thoracic kyphosis (rounded upper back), and performing repetitive motions (specifically extension of the lumbar spine).
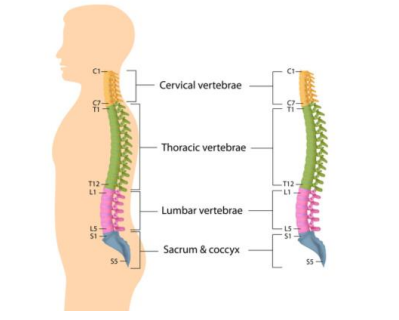
To understand more about back injuries, we have to learn about the anatomy. The back is made up of bones (vertebrae), muscles, tendons, ligaments, vertebral discs, nerves, and more. The cervical spine has 7 vertebrae and makes up your neck. The thoracic spine has 12 vertebrae and connects to the ribs. The lumbar spine has 5 vertebrae and makes up your low back. There are vertebral discs between each of the vertebrae and the discs help absorb force from landing and pounding.
If back pain is occurring in your gymnast, you should seek medical attention. During the medical visit a physical exam will be performed, and sometimes diagnostic tests may be ordered. These tests may include an x-ray, MRI, CT scan, or possibly a bone scan.
Once you have been seen by a medical provider you will be given a diagnosis or reason for your back pain. The most common causes of back pain in gymnasts are spondylolysis, spondylolisthesis, discogenic back pain, and mechanical/gymnast back pain (3).
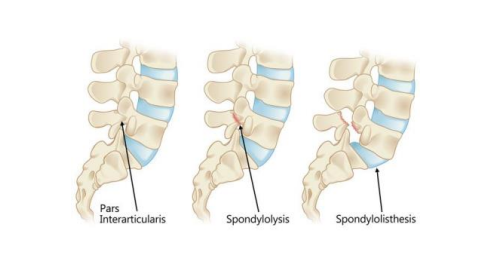
Spondylolysis is a stress fracture or fracture of an area of the vertebra, mostly commonly in the low back, and occurs from repetitive hyperextension (arching backwards) and rotation of the lumbar spine (1,3). Preventable risk factors to have a spondylolysis include, but are not limited to, lacking shoulder flexion, reduced thoracic mobility, reduced hip extension mobility, hinging from your lumbar spine, decreased core strength, and sports/skills with repetitive hyperextension (arching backwards) (3). Gymnasts may explain that they have pain with arching/extension skills such as bridges, back walkovers, and back handsprings in the low back. A medical provider may order a variety of diagnostic tests to understand your back pain and where the spondylolysis is occurring. When a gymnast has a bilateral spondylolysis (fractures on both sides of the vertebra), and the vertebra starts to slide forward this is called spondylolisthesis.
Discogenic back pain is an injury to the disc of the spine and typically occurs in an adolescent or young adult gymnast, or a gymnast with a history of having a spondylolisthesis. It most commonly occurs in the lumbar spine and risk factors for having discogenic back pain include, but are not limited to, sports with repetitive hyperflexion (bending forward), and a history of a previous back injury (3). This typically occurs from repetitive flexion of the spine causing the disc to be pinched or squeezed. Gymnasts typically explain that they have pain with flexion-based skills, sometimes have tingling or pins and needles down their leg, and their pain is worse when they sneeze, cough, or strain. If this injury is suspected, you should see a medical provider and diagnostic tests may be ordered.
Mechanical/Gymnast low back pain is any type of back pain caused by placing abnormal stress and strain on the back and is a diagnosis of exclusion (meaning everything else was ruled out by a medical provider) (3). This can occur in any gymnast and at any age. Risk factors for mechanical/gymnast low back pain include, but are not limited to, decreases in shoulder flexion, thoracic mobility, hip extension, and core strength, and sports with repetitive hyperflexion (bending forward) and hyperextension (arching backward), and a history of previous back injury. Because this is a diagnosis of exclusion your medical provider may order several diagnostic tests.
Once you have been cleared by a medical provider it is important to follow the below steps with your progression back to gymnastics:
• Obtain clearance from a medical provider to go back to gymnastics
• Go slow
• However long you are out, is how long you should take to get back all of your skills
• Listen to your body
• Consider changing elements in your routine – eg if your gymnast has a spondylolysis and extension-based skills caused her injury, consider removing extension-based skills until a later date/farther out from the injury date
• Prevention, Prevention, Prevention (see the next paragraph)
• Have a plan in place and include the gymnast, parent, coaches, and medical team
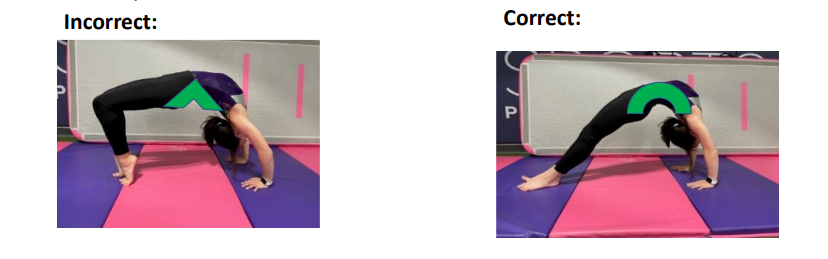
Prevention is key to avoid back pain. Studies have shown that working on core stabilization/strength, increasing thoracic spine mobility, fixing posture, increasing hip flexor flexibility, and increasing gluteus and periscapular strength can decrease back pain and injuries (1, 3, 4). Other ways to decrease back pain is to look at the “hinge point”-where a gymnast is bending or hinging from (4). Gymnasts should be using their entire spine to arch backwards and flex forward. The back bend should look like a true arch and not an upside-down “V” (see below).
In summary, gymnasts who experience back pain should be seen by a medical provider, the most common causes of back pain are spondylolysis, spondylolisthesis, discogenic back pain, and mechanical/gymnast back pain, and prevention is key to avoid back pain and injury.
References:
1. Spine Injuries in the Sport of Gymnastics. David Kruse, MD and Brooke Lemmen, MD
2. Lumbar Spine Injuries in National Collegiate Athletic Association Athletes A 6-
Season Epidemiological Study. Jeffrey D. Hassebrock, MD, et. al.
3. The Young Injured Gymnast: A Literature Review and Discussion. Elspeth Hart, PAC, ATC; William P. Meehan III, MD; Donald S. Bae, MD; Pierre D’Hemecourt, MD,
FACSM; and Andrea Stracciolini, MD, FACSM
4. Stretching the Spines of Gymnasts: A Review. William A. Sands, et. al.
Dr. Elly Hart, DScPAS, PA-C, MPAS, ATC, LAT is a Physician Assistant at Boston Children’s Hospital and founder of Gymnastics Medicine: Education and Research.
Original blog post can be found in the October 2022 USA Gymnastics Newsletter: https://usagym.org/PDFs/About%20USA%20Gymnastics/wellness/backpain.pdf